Papillary Mesothelioma
Papillary mesothelioma is a rare form of epithelial mesothelioma. It may occur in the linings of the abdomen (peritoneum), lungs (pleura) or testicles (tunica vaginalis). In general, it is benign and has a favorable prognosis. It is also called well-differentiated papillary mesothelioma (WDPM).
What Is Papillary Mesothelioma?
Papillary mesothelioma, also called well-differentiated papillary mesothelioma (WDPM), is a rare subtype of epithelial mesothelioma. It most often occurs in the lining of the abdomen (peritoneum). Less often, it may occur in the linings of the lungs (pleura) or testicles (tunica vaginalis).
Characteristics of papillary mesothelioma include:
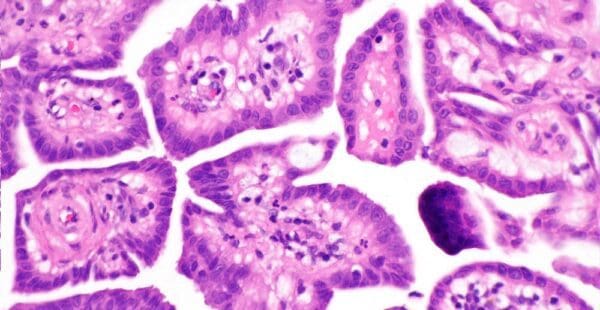
- Cell growth: WDPM cell growth is slow and microscopic. This growth pattern differentiates epithelial mesothelioma from malignant sarcomatoid mesothelioma. In contrast, sarcomatoid cells exhibit aggressive behavior and rapid growth.
- Cell pattern: WDPM cells can be round or oval. The cells form finger-like projections called papillae.
- Patient demographic: WDPM is most common in young women, especially those with a history of endometriosis and ovarian cancer.
- Tumor location: Papillary mesothelioma affects cells in the linings of internal organs.
- Unique calcification: In rare cases, papillary cancers may form psammoma bodies. Psammoma bodies are areas of calcification within the tumor.
Identifying tumor cell characteristics can help differentiate papillary mesothelioma from other mesothelioma subtypes.
Is Papillary Mesothelioma Benign?
Papillary mesothelioma is typically benign.
Some researchers have reported WDPM becoming malignant over a period of years. However, others have concluded WDPM is not a precursor to malignant mesothelioma. Conflicting information may be due to initial misdiagnosis of malignant mesothelioma as WDPM.
WDPM does not usually recur after it is treated because it is normally benign. Patients often experience no symptoms and live many years with this condition.
Request a Free 2026 Mesothelioma Guide Our packet will be sent to you within 24 hours Request Free GuideWell-Differentiated Papillary Mesothelioma and Asbestos
Papillary mesothelioma has been linked to asbestos exposure. In a review of 24 pleural WDPM cases, half of the patients had confirmed occupational asbestos exposure.
Published cases of papillary mesothelioma are rare. The disease is prone to misdiagnosis or being left undiagnosed altogether. These factors make the condition difficult to study.
Asbestos exposure itself is also difficult to track. Occupational asbestos exposure is the most common cause of mesothelioma. However, individuals may be exposed at home, school and many other locations.
It is difficult to measure how often people exposed to asbestos develop papillary mesothelioma because there is so little data.
Papillary Mesothelioma Symptoms
The majority of patients diagnosed with papillary mesothelioma show no symptoms.
One MD Anderson Cancer Center study reviewed 26 female patients with papillary mesothelioma. In this study, only two patients presented symptoms. However, any reported symptoms can help physicians reach an accurate diagnosis.
- Abdominal pain
- Bloating (peritoneal effusion)
- Pelvic mass
- Pelvic pain
- Collapsed lung (pneumothorax)
- Inflammation of the pleura and pericardium (pleuropericarditis)
- Pleural effusion
- Pleural thickening
- Shortness of breath (dyspnea)
- Fluid-filled sac around scrotum (hydrocele)
- Scrotal nodules
- Scrotal swelling
Diagnosing Well-Differentiated Papillary Mesothelioma
Papillary mesothelioma diagnosis often occurs incidentally during other procedures. This means doctors often find it when performing other procedures on a patient.
However, well-differentiated papillary mesothelioma can be discovered in several ways, including:
- Biopsies: Tissue biopsies may help diagnose WDPM. These include laparoscopic biopsy, open biopsy and thoracoscopic biopsy.
- Histology and pathology: Microscopic analysis of biopsy samples can identify WDPM.
- Imaging scans: X-rays and CT scans can help identify WDPM tumors.
- Immunohistochemistry: This process uses special dyes to identify unique cell proteins.
These methods may be combined to confirm a diagnosis. However, biopsies are the only way to definitively diagnose papillary mesothelioma. A biopsy can characterize tumor cells, including mesothelioma type and stage. Biopsies are crucial for an accurate diagnosis. They can also help prevent cancer misdiagnosis.
Papillary mesothelioma is prone to misdiagnosis. In part because of its rarity, doctors may mistake WDPM symptoms for signs of other conditions, including:
- Acute cholecystitis
- Appendicitis
- Clear cell carcinoma
- Incarcerated umbilical hernia
- Ovarian cancer
- Ovarian sex cord tumor
- Papillary serous carcinomas
Patients who know they have a history of asbestos exposure should tell their doctors. This can help doctors make accurate diagnoses.
To prevent misdiagnosis, physicians may also observe symptoms and common co-occurring conditions.
Conditions associated with papillary mesothelioma include:
- Colorectal cancer
- Endometriosis
- Ovarian cancer
The presence of the conditions in conjunction with WDPM has been observed in a few patients. There is not enough data for the conditions to be considered risk factors for mesothelioma. However, they may assist doctors with correctly diagnosing papillary mesothelioma.
Accurate diagnosis is important to ensure the disease is treated correctly.
What Is the Prognosis for Papillary Mesothelioma?
WDPM is typically benign and has a very favorable mesothelioma prognosis. Patients may survive for years or decades. The most common type of WDPM, which affects the peritoneum, has a 5-year survival rate of 90% with treatment. This means that about 90% of patients are still alive 5 years after diagnosis.
In the MD Anderson Cancer Center study of 26 papillary mesothelioma patients:
- 22 survived with no recurrence
- 1 patient experienced recurrence of WDPM after four years
- 3 patients died of other causes
Papillary mesothelioma has a low malignant potential. However, because research on WDPM is limited, long-term follow-ups and monitoring are recommended.
How Is Papillary Mesothelioma Treated?
Treatment is not always required for benign WDPM. However, treatment options for papillary mesothelioma may include:
- Surgical removal of the tumor
- Cytoreductive surgery (CRS)
- Hyperthermic intraperitoneal chemotherapy (HIPEC)
- Early postoperative intraperitoneal chemotherapy (EPIC)
- Immunotherapy
- Multimodal treatment
Treatment for well-differentiated papillary mesothelioma depends on malignancy. Benign mesothelioma tumors are typically removed with complete surgical resection.
Treatment for WDPM may include chemotherapy drugs such as cisplatin, doxorubicin and oxaliplatin.
However, researchers in one study of peritoneal WDPM noted that post-surgical chemotherapy “does not seem to bring added value” to treatment regimens. Researchers suggest patients with inoperable tumors be monitored for progression rather than attempting more aggressive treatments.
Researchers in a study of pleural WDPM found no evidence suggesting chemotherapy or radiation were beneficial.
Ultimately, more research is needed for a standard treatment plan for papillary mesothelioma. Patients should seek professional medical advice to establish an individualized mesothelioma treatment plan.
Questions About Papillary Mesothelioma? Ask experienced mesothelioma advocate Jennifer Lucarelli Ask a QuestionCommon Questions About Papillary Mesothelioma
How is a well-differentiated papillary mesothelial tumor treated?
What is the prognosis for papillary mesothelioma?
What is well-differentiated papillary mesothelioma of the stomach?
What is the survival rate for malignant papillary mesothelioma?
Sources
Baker PM, Clement PB, et al. Malignant Peritoneal Mesothelioma in Women: A Study of 75 Cases With Emphasis on Their Morphologic Spectrum and Differential Diagnosis. American Journal of Clinical Pathology. May 2005;123(5):724-737. doi: 10.1309/2h0n-vrer-pp2l-jdua
Bridda A, Padoan I, et al. Peritoneal Mesothelioma: A Review. Medscape General Medicine. May 2007;9(2):32.
Bürrig KF, Pfitzer P, et al. Well-differentiated papillary mesothelioma of the peritoneum: A borderline mesothelioma. Virchows Archiv A, Pathological Anatomy and Histopathology. September 1990;417(5):443-447. doi: 10.1007/BF01606033
Chen X, Sheng W, et al. Well-differentiated papillary mesothelioma: a clinicopathological and immunohistochemical study of 18 cases with additional observation. Histopathology. April 2013;62(5):805-813. doi: 10.1111/his.12089
Erem AS, Allamaneni SS, et al. Well-Differentiated Papillary Mesothelioma with Omental Calcifications: A Case Report and Review of the Literature. American Journal of Case Reports. January 2020;21:e920487-1-e920487-9. doi: 10.12659/AJCR.920487
Galateau-Sallé F, Vignaud JM, et al. Well-differentiated papillary mesothelioma of the pleura: a series of 24 cases. American Journal of Surgical Pathology. April 2004;28(4):534-540. doi: 10.1097/00000478-200404000-00013
García-Fadrique A, Mehta A, et al. Clinical presentation, diagnosis, classification and management of peritoneal mesothelioma: a review. Journal of Gastrointestinal Oncology. October 2017;8(5):915-924. doi: 10.21037/jgo.2017.08.01
Huang Y-T, Huang H-Y, et al. Paratubal Well-differentiated Papillary Mesothelioma. Journal of Minimally Invasive Gynecology. May-June 2020;27(4):805-806. doi: 10.1016/j.jmig.2019.08.023
Malpica A, Sant’Ambrogio S, et al. Well-differentiated papillary mesothelioma of the female peritoneum: a clinicopathologic study of 26 cases. American Journal of Surgical Pathology. January 2012;36(1):117-127. doi: 10.1097/PAS.0b013e3182354a79
Park JY, Kim KW, et al. Peritoneal mesotheliomas: clinicopathologic features, CT findings, and differential diagnosis. AJR American Journal of Roentgenology. September 2008;191(3):814-825. doi: 10.2214/AJR.07.3628
Shrestha R, Nabavi N, et al. Well-Differentiated Papillary Mesothelioma of the Peritoneum Is Genetically Distinct from Malignant Mesothelioma. Cancers (Basel). June 2020;12(6):1568. doi: 10.3390/cancers12061568
Stevers M, Rabban JT, et al. Well-differentiated papillary mesothelioma of the peritoneum is genetically defined by mutually exclusive mutations in TRAF7 and CDC42. Modern Pathology. January 2019;32(1):88-99. doi: 10.1038/s41379-018-0127-2
Sun M, Zhao L, et al. Well-differentiated papillary mesothelioma: A 17-year single institution experience with a series of 75 cases. Annals of Diagnostic Pathology. February 2019;38:43-50. doi: 10.1016/j.anndiagpath.2018.10.012
Vogin G, Hettal L, et al. Well-Differentiated Papillary Mesothelioma of the Peritoneum: A Retrospective Study from the RENAPE Observational Registry. Annals of Surgical Oncology. March 2019;26(3):852-860. doi: 10.1245/s10434-018-07153-2
Wang X, Ren W, et al. A giant, well-differentiated papillary mesothelioma of the left atrioventricular groove: Case report and brief review of the literature. Journal of Clinical Ultrasound. November 2019;47(9):564-567. doi: 10.1002/jcu.22730

Katy Moncivais, Ph.D., has more than 15 years of experience as a medical communicator. As the Medical Editor at Mesothelioma.com, she ensures our pages and posts present accurate, helpful information.
Dr. James Stevenson is a Board-Certified Medical Oncologist. He specializes in treating mesothelioma and lung cancer and practices at the Cleveland Clinic in Cleveland, Ohio.
